BRAINCELL: Pioneering a Liquid Biopsy for Brain Metastases
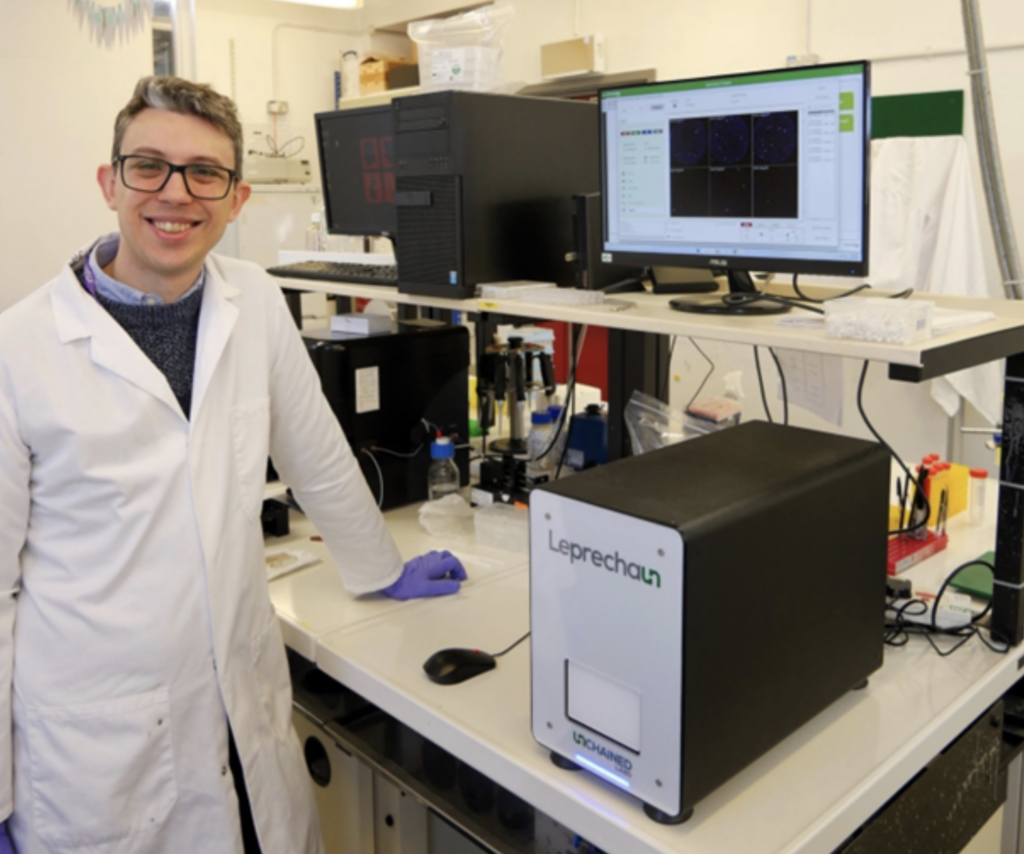
Sussex Cancer Fund is proud to be supporting this ambitious and potentially life-changing project with £60,000 of funding. We’re joining forces with Action Against Cancer, who are also generously contributing £60,000 awarded to Professor Georgios Giamas, Professor of Cell Signalling at the University of Sussex, with the project lead Dr Stephen Robinson. Together, we’re helping to make this important research happen.
What’s the problem?
Brain metastases (when cancer spreads to the brain) are a serious and often life-limiting development for many people living with cancer. They are especially common in individuals with lung cancer, melanoma, and certain types of breast cancer. At the moment, there’s no way to predict who will develop brain metastases, and diagnosis often means undergoing risky brain surgery. Even after diagnosis, regular MRI scans are used to check if the cancer has come back—but these are expensive, sometimes inconclusive, and can be very stressful for patients and families.
Our solution: a blood test instead of brain surgery
The BRAINCELL research project, led by Dr Stephen Robinson at the University of Sussex and supported by a team of national and international collaborators, is working to develop a revolutionary liquid biopsy, a simple blood test to detect and monitor brain metastases.
By focusing on tiny particles in the blood called extracellular vesicles, the team hopes to find a reliable way to diagnose brain metastases, predict outcomes, guide treatment, and monitor for recurrence, all from a routine blood test.
Why this research matters
This is a unique, internationally-leading research project with the potential to completely transform how we care for people with cancer who are at risk of brain metastases. It is:
- Patient-focused – developed with guidance from people living with cancer.
- Non-invasive – no need for brain surgery or repeated MRI scans.
- Personalised – helping clinicians tailor treatments to the individual.
- Predictive – potentially spotting recurrence early, when it’s most treatable.
Collaboration across the UK, and beyond
This exciting project is based at the University of Sussex and brings together a wide range of experts and institutions. The Royal Marsden Hospital is playing a key role by supporting patient recruitment and treatment. The University of Manchester, Teesside University, and the University of Otago in New Zealand are lending their expertise in advanced data analysis and biomarker validation. It’s also supported by international research groups and networks, all working together to improve care for people living with brain tumours. This strong collaboration means we can share knowledge, speed up discoveries, and make sure the results have global relevance.
What will happen during the study?
Around 70 patients with brain metastases will take part in the study. Blood samples will be collected at several points during their treatment. These samples will then be carefully analysed in the lab, focusing on tiny particles called extracellular vesicles. By looking at the protein and RNA markers within these particles, researchers hope to discover reliable “biomarker signatures” that could reveal the presence of brain metastases, help track treatment response, and monitor for recurrence. These findings could then be tested and validated in future studies.
When will this help patients?
The ultimate goal of this research is to develop a simple blood test that can diagnose brain metastases, predict who will benefit most from treatment, and detect any return of the disease early. While turning research into everyday clinical practice takes time, the team hopes that, with successful early results, a follow-up clinical trial could begin within two years. If all goes well, this test could be ready to use in clinics within the next five to seven years.


